In recent years, U.S. maternal mortality has emerged as a pressing public health crisis, with the country leading high-income nations in pregnancy-related deaths. Alarmingly, more than 80 percent of these fatalities are deemed preventable, raising critical questions about the effectiveness of current prenatal and postpartum care systems. Disparities in maternal health highlight profound inequities across states, races, and ethnicities, underscoring the urgent need for attention to the risks of maternal mortality. A comprehensive approach to improving prenatal care and understanding postpartum care importance is essential to curtail these preventable pregnancy deaths. By focusing on these key areas and addressing maternal health disparities, the U.S. can create a more equitable healthcare landscape for all mothers.
The alarming rise in pregnancy-related deaths in America highlights a severe maternal health crisis that warrants immediate attention. With a disproportionate impact on marginalized racial and ethnic groups, the situation reveals significant gaps in care that contribute to preventable fatalities. Many factors contribute to this issue, including inadequate access to quality healthcare and chronic health conditions exacerbated by systemic disparities. Fostering better prenatal services and extending comprehensive postpartum care can play a pivotal role in improving health outcomes. It’s essential for policymakers and healthcare providers to work collaboratively to combat the troubling statistics surrounding maternal well-being in the United States.
Understanding U.S. Maternal Mortality Rates
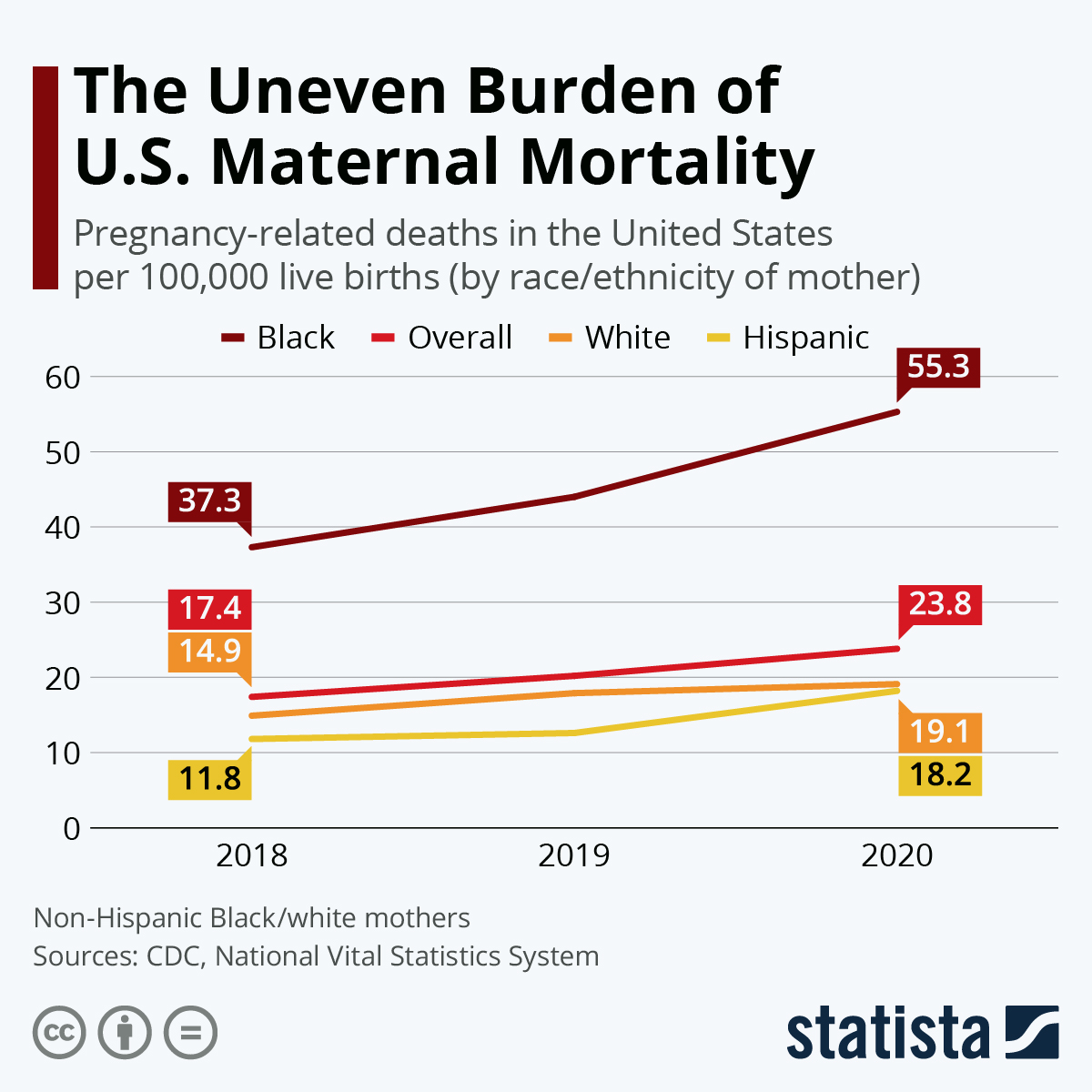
Maternal mortality rates in the U.S. have been a growing concern, particularly as the nation continues to report the highest numbers among high-income countries. A recent study indicated that the U.S. maternal mortality rate increased significantly between 2018 and 2022, with alarming disparities affecting women of different races and ethnicities. Notably, American Indian and Alaska Native women experienced the highest rates of pregnancy-related deaths, pointing to a widespread issue that extends beyond just healthcare access. This situation indicates systemic issues within the U.S. healthcare system that require urgent attention and reform.
Understanding the factors contributing to these high maternal mortality rates is crucial. Previous research has highlighted the role of chronic health conditions, inadequate prenatal care, and disparities in healthcare access as primary drivers of preventable pregnancy deaths. Additionally, the ongoing impact of the COVID-19 pandemic exacerbated these challenges, with many expecting mothers facing heightened risks. As experts like Associate Professor Rose Molina indicate, addressing these challenges necessitates a comprehensive review of healthcare policies, particularly those aimed at improving maternal health outcomes across various demographics.
Preventable Pregnancy Deaths: A Call to Action
The shocking reality is that over 80 percent of pregnancy-related deaths in the U.S. are preventable. This statistic serves as a clarion call for action regarding maternal health policies and practices. By identifying and addressing the primary causes of maternal mortality, especially cardiovascular diseases that have become the leading cause, stakeholders can reverse this troubling trend. Enhancing prenatal care through better education, resources, and access to healthcare professionals can significantly reduce these deaths.
Furthermore, for change to occur, awareness must extend beyond immediate prenatal care and include postpartum care importance. Many women experience complications well after childbirth, with one-third of maternal deaths occurring between 42 days to one year later. This highlights the necessity for comprehensive healthcare that spans the entirety of the maternal experience, encouraging increased visits and support in the postpartum phase. Public health initiatives and community programs can play a vital role in addressing the existing disparities and decreasing the number of preventable deaths.
Maternal Health Disparities in America
Maternal health disparities in the U.S. are stark, illustrating a troubling divide based on race and geography. American Indian and Alaska Native women face dramatically higher maternal mortality rates, a statistic that reveals the intersection of healthcare inequalities and systemic biases. Additionally, the variations in state-level outcomes underscore the need for targeted interventions that address these disparities. Every state should strive for the success seen in states like California, which have demonstrated that a reduction in maternal deaths is achievable through comprehensive policy initiatives.
To tackle these disparities effectively, healthcare systems must better understand and address the specific needs of at-risk populations. Investments in community-based support services are critical, including culturally competent care that respects and understands the unique challenges faced by these communities. Furthermore, resolving disparities demands collaboration across healthcare sectors, government agencies, and community organizations to foster an environment where every mother, regardless of background, has access to quality prenatal and postpartum care.
Improving Prenatal Care Systems
Improving prenatal care systems is fundamental to reducing maternal mortality rates in the U.S. Access to quality prenatal care is not universally available, which exacerbates maternal health disparities across different regions and demographics. Innovative approaches, such as integrating telehealth services, can bridge the gap for underserved communities. Through early and consistent prenatal visits, healthcare providers can monitor potential complications more effectively, allowing for timely interventions that are critical to maternal health.
Moreover, educational initiatives aimed at expectant mothers are crucial. Women should receive comprehensive information about the warning signs of complications, pregnancy risks, and the importance of regular check-ups. By empowering women with knowledge about their health and encouraging proactive engagement with healthcare providers, the chances of identifying issues early can significantly increase, thereby enhancing overall maternal health outcomes and reducing the number of preventable pregnancy deaths.
The Importance of Postpartum Care
Postpartum care is an often overlooked yet vital component of maternal health. Many healthcare systems in the U.S. focus primarily on prenatal visits, neglecting the importance of support and care during the postpartum period. This lack of emphasis can lead to dangerous outcomes, as complications can arise long after delivery. Late maternal deaths, which occur between 42 days and one year post-birth, account for nearly one-third of maternal deaths, highlighting the significant gap in care that needs to be addressed.
To improve postpartum care, there needs to be a cultural shift within healthcare toward recognizing the postpartum period as a continuum of care rather than a separate, less critical phase. Maternal health policies should include structured follow-ups and support services that extend well into the year after childbirth. Ensuring that mothers receive the necessary medical, emotional, and psychological support could drastically lower maternal mortality rates and improve long-term health outcomes for mothers and their babies.
Intersection of Chronic Health Conditions and Pregnancy
Chronic health conditions, such as hypertension and heart disease, significantly influence maternal mortality rates, especially among younger women. Recent findings reveal that women aged 25 to 39 are increasingly affected by these conditions, which previously predominantly impacted older populations. As chronic illnesses become more prevalent among reproductive-age individuals, it is essential for healthcare providers to address these issues early through education and monitoring.
Integrating chronic disease management into prenatal care can help mitigate risks associated with pregnancy and childbirth. For instance, appropriately managing hypertension can prevent severe complications and enhance maternal outcomes. Additionally, ongoing education for healthcare providers on recognizing and addressing chronic conditions within the context of pregnancy can lead to better health interventions from early pregnancy all the way through the postpartum phase.
Racial and Ethnic Inequities in Maternal Health
The racial and ethnic inequities present in maternal health outcomes in the U.S. are striking. Research consistently shows that women of color, particularly Black and Native American women, experience much higher rates of maternal mortality compared to their white counterparts. These disparities result from a combination of systemic factors, including access to quality healthcare, levels of social support, and existing health conditions. Addressing these issues requires not only improved healthcare access but also an examination of racial biases within medical practices that can adversely affect care quality.
To combat these inequities, it is crucial to implement training for healthcare providers to recognize implicit biases and its impacts on patient care. Furthermore, emphasizing community health initiatives that target high-risk groups can facilitate a more supportive environment for these populations. Programs that provide education, resources, and proactive healthcare can help empower marginalized communities and lead to better maternal health outcomes.
The Role of Public Health Infrastructure
The public health infrastructure plays a pivotal role in addressing the rising rates of maternal mortality in the U.S. There is a pressing need for continuous investment in public health initiatives focused on improving maternal health outcomes. This support enables the development of programs that provide essential services, resources, and education to women before, during, and after pregnancy. It is imperative to recognize the importance of robust infrastructure to ensure effective tracking and reporting of maternal health statistics.
Additionally, any cuts to public health funding can have detrimental effects on maternal health efforts. Sustained support is necessary for research that informs policy changes and advocates for improved access to care. Engaging stakeholders across various sectors, including public health, healthcare providers, and community organizations, can amplify the impact of these efforts, creating a multi-faceted approach to reducing maternal mortality.
Advocating for Policy Reforms in Maternal Health
Advocating for comprehensive policy reforms in maternal health is crucial for addressing the rising rates of pregnancy-related deaths. Effective reforms can improve access to essential services, particularly for underserved populations. Policymakers must prioritize maternal health issues by investing in programs that enhance prenatal and postpartum care, as well as by addressing the systemic inequities seen across state lines. This collaborative approach can help standardize care levels and ensure that all women receive the attention they need during this critical time.
Moreover, involving communities in discussions about maternal health reforms is essential for tailoring solutions that meet local needs. Policy advocacy should focus on building coalitions between healthcare providers, community organizations, and mothers to ensure that the voices of those most affected are heard. These collaborative efforts can drive effective legislative changes that prioritize maternal health and ultimately work towards achieving better outcomes for all mothers.
Frequently Asked Questions
What are the primary causes of U.S. maternal mortality?
The leading cause of U.S. maternal mortality is cardiovascular disease, which includes conditions such as hypertension, pre-eclampsia, and cardiac disorders. Additionally, preventable pregnancy deaths often stem from systemic inequities in healthcare access and the prevalence of chronic health issues among pregnant individuals.
How can improving prenatal care reduce maternal mortality in the U.S.?
Enhancing prenatal care is vital in reducing U.S. maternal mortality as it helps identify health risks early, provides essential screenings, and educates expectant mothers about their health. Comprehensive prenatal care can significantly decrease risks of complications that lead to preventable pregnancy deaths.
What are the maternal health disparities contributing to higher mortality rates in the U.S.?
Maternal health disparities in the U.S. result from systemic inequities in healthcare that affect various groups disproportionately. Racial and ethnic minorities, particularly American Indian, Alaska Native, and non-Hispanic Black women, experience higher rates of maternal mortality due to factors like biased treatment in healthcare and limited access to appropriate maternity care.
Why is postpartum care important for preventing maternal mortality?
Postpartum care is critical because nearly one-third of maternal deaths occur between 42 days and one year after pregnancy. Continuity of care during this period can address health issues that arise after childbirth, therefore, improving overall maternal health outcomes and reducing the risks of late maternal deaths.
What role does addressing chronic health issues play in reducing the risks of maternal mortality?
Addressing chronic health issues, such as hypertension and diabetes, is essential in reducing risks of maternal mortality in the U.S. As more individuals experience chronic conditions at younger ages, effective management and treatment during pregnancy can lower complications and prevent preventable pregnancy deaths.
How does the U.S. maternal mortality rate compare to other high-income countries?
The U.S. has the highest maternal mortality rate among high-income countries, with significant disparities based on state, race, and ethnicity. Continuous rises in these rates reveal the critical need for improved maternal healthcare systems and policies alike to ensure every mother receives the care they need.
What measures can be taken to improve maternal health outcomes in the U.S.?
Improving maternal health outcomes in the U.S. requires investing in quality prenatal and postpartum care, addressing policy disparities among states, and increasing access to comprehensive healthcare services that consider the unique needs of pregnant individuals to tackle the root causes of preventable pregnancy deaths.
| Key Point | Details |
|---|---|
| Preventable Deaths | Over 80% of pregnancy-related deaths in the U.S. are preventable. |
| High Rates | The U.S. has the highest maternal mortality rate among high-income countries, which has continued to rise from 2018 to 2022. |
| Racial Disparities | Significant disparities exist in maternal mortality rates among racial and ethnic groups. American Indian and Alaska Native women have the highest rates. |
| Primary Causes | Cardiovascular disease is the leading cause of pregnancy-related death, which has shifted from hemorrhage over decades. |
| COVID-19 Impact | The COVID-19 pandemic correlated with a rise in pregnancy-related deaths, peaking in 2021. |
| Need for Comprehensive Care | Calls for better prenatal and postpartum care, emphasizing that late maternal deaths significantly contribute to mortality rates. |
| Public Health Infrastructure | Investment in public health infrastructure is crucial for improving maternal health outcomes. |
Summary
U.S. maternal mortality is a growing concern, with preventable deaths rising over recent years. The statistics reveal urgent disparities in maternal care, highlighting the need for improved healthcare systems and resources. With a significant proportion of these deaths being avoidable, it is imperative for policymakers to address the underlying issues within the current healthcare framework to ensure equitable and quality care for all women during and after pregnancy.