TIM-3 therapy for Alzheimer’s offers a groundbreaking approach to addressing the challenges of Alzheimer’s disease treatment. This innovative strategy involves targeting the TIM-3 checkpoint molecule, which plays a crucial role in the immune response within the brain. Recent studies have shown that inhibiting TIM-3 can reactivate microglia, the brain’s immune cells, enabling them to effectively clear amyloid plaques associated with cognitive decline. By improving cognitive function and memory retention in experimental models, TIM-3 therapy illustrates the potential for repurposing immune system cancer therapy to combat neurodegeneration. As researchers delve deeper into this promising area, the implications of TIM-3 therapy could revolutionize the landscape of Alzheimer’s disease treatment and provide hope for millions affected by this debilitating condition.
The TIM-3 checkpoint molecule emerges as a pivotal target in the search for effective Alzheimer’s therapies, opening new avenues for intervention in neurodegenerative diseases. By understanding microglial behavior and their critical role in maintaining cognitive health, scientists are exploring ways to modify immune responses to combat amyloid plaque buildup. This potential treatment methodology seeks to enhance the natural abilities of immune cells within the brain, thereby addressing cognitive decline directly. Utilizing anti-TIM-3 antibodies, researchers aim to harness the immune system’s power, echoing similar strategies found in successful immune system cancer therapies. The exploration of these concepts marks a significant shift in how we view Alzheimer’s pathology and treatment, emphasizing the need for innovative, targeted interventions.
Understanding TIM-3 and Alzheimer’s Disease
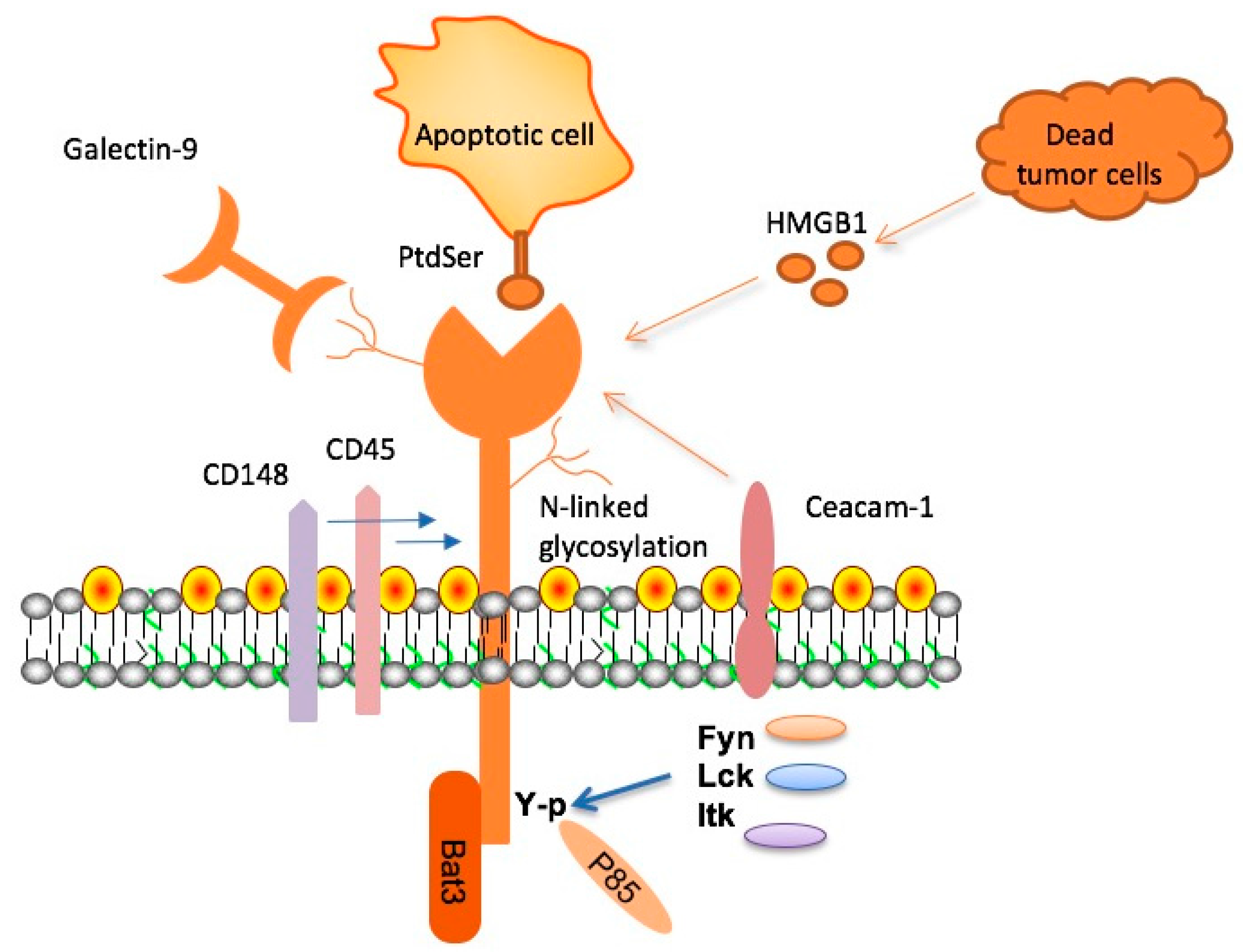
TIM-3, or T cell immunoglobulin and mucin domain-3, is a checkpoint molecule that has gained attention for its role in Alzheimer’s disease (AD). This molecule typically serves to inhibit the immune response, preventing aggressive actions by T cells that could harm the body. However, in the context of AD, TIM-3’s action actually leads to dysfunctional microglia, the brain’s immune cells, which become incapable of clearing amyloid plaques. Research shows that TIM-3 is significantly upregulated in the microglia of Alzheimer’s patients, reinforcing its role as a key player in the progression of the disease.
The importance of TIM-3 in late-onset Alzheimer’s is underscored by genetic studies linking the HAVCR2 gene—which codes for TIM-3—to the disease. This connection suggests that individuals with certain genetic polymorphisms may have an increased risk for developing Alzheimer’s due to TIM-3’s influence on immune regulation in the brain. By understanding how TIM-3 hinders microglial activity, researchers hope to find new therapeutic strategies that can enhance cognitive function by targeting this molecule.
Microglia: The Immune Guardians of the Brain
Microglia represent the primary immune cells in the brain and play a crucial role in maintaining both brain health and cognitive function. These cells are responsible for eliminating waste and dead neurons through a process known as phagocytosis. However, as Alzheimer’s disease progresses, microglia become ‘homeostatic’ due to factors like TIM-3, preventing them from effectively clearing accumulated plaques. Without the necessary action from microglia, these plaques can accumulate, leading to further cognitive decline.
In a healthy brain, microglial cells engage in clearing synaptic debris, which is vital for memory retention and cognitive agility. Yet, in the presence of Alzheimer’s, the microglial response is impaired. This dysfunction not only contributes directly to plaque accumulation but also affects the brain’s overall ability to adapt and maintain cognitive functions. Understanding this dynamic opens pathways for potential interventions, such as TIM-3 therapy, that may reactivate microglial activities to combat the disease.
The Promise of Anti-TIM-3 Antibodies
The development of anti-TIM-3 antibodies presents a novel approach to Alzheimer’s treatment. By inhibiting the function of TIM-3, these antibodies aim to rejuvenate the microglial response, allowing for the clearance of amyloid plaques from the brain. In laboratory studies, animals treated with TIM-3 inhibitors demonstrated notable cognitive improvements, highlighting the potential efficacy of this therapeutic approach. This reflects a significant shift in how we might approach Alzheimer’s treatment, leaning towards immunotherapy—a strategy that has proven successful against various cancers.
This approach is particularly promising considering the limitations of traditional treatments that primarily target amyloid beta. Anti-TIM-3 therapies could offer a more effective means to not only reduce plaque burden but also enhance overall cognitive function. With ongoing research focusing on human trials and the safety profiles of these antibodies, the potential for developing TIM-3 therapy for Alzheimer’s could bridge gaps left by previous treatment failures.
Challenges in Alzheimer’s Disease Treatment
Despite advancements in understanding Alzheimer’s disease pathology, effective treatments remain elusive. Traditional therapies have often resulted in only marginal cognitive improvement, indicating a need for more targeted approaches. One significant challenge is that amyloid plaques are not only present in the brain but also appear in blood vessels, complicating treatment efficacy. This has led to some therapies causing vascular complications, which can worsen patient outcomes and limit their use in clinical settings.
Researchers are now exploring how selective targeting of proteins like TIM-3 can bypass these complications. By focusing on mechanisms that activate microglia, such as the inhibition of TIM-3, scientists are hopeful that new treatments can facilitate the natural clearance of plaques without adversely affecting the vascular system. Innovative approaches like this are crucial in overcoming the hurdles faced in Alzheimer’s disease management.
Cognitive Function Improvement Through Microglial Activation
Enhancing cognitive function in Alzheimer’s patients is a pivotal goal in ongoing medical research. Studies indicate that by targeting the microglial cells—specifically through the modulation of TIM-3 expression—there is potential for significant cognitive restoration. For instance, experiments with genetically modified mice lacking the TIM-3 gene showed not only reduced plaque accumulation but also improved memory and navigational skills in behavioral tests, suggesting a clear link between microglial function and cognitive health.
The concept of cognitive function improvement through microglial activation emphasizes a shift away from merely addressing symptoms towards modifying disease progression. Timely intervention that promotes microglial health and function may yield better outcomes for patients, leading to longer periods of cognitive vitality. Future clinical trials will be instrumental in confirming these findings in human subjects and may pave the way for new standards in Alzheimer’s treatment.
The Role of Immunotherapy in Alzheimer’s Management
Immunotherapy has changed the landscape of cancer treatment and holds promise for neurodegenerative diseases like Alzheimer’s. By leveraging the body’s immune system to combat the pathology associated with Alzheimer’s, targeted therapies such as anti-TIM-3 antibodies represent a new frontier. These therapies aim to re-engage the immune response within the brain, facilitating the clearance of harmful amyloid plaques that contribute to cognitive decline, ultimately improving memory and learning capabilities.
This innovative approach aligns with findings from various studies indicating that the immune system, when properly activated, can enhance neuroprotection and promote cognitive resilience. However, it also underscores the need for tailored therapies that consider the unique challenges faced in treating Alzheimer’s compared to other conditions. As research progresses, immunotherapy will likely become an integral part of comprehensive Alzheimer’s care strategies.
Ongoing Research in Alzheimer’s Therapy
Research into Alzheimer’s therapies, particularly those targeting TIM-3, is actively progressing across multiple fronts. Scientists are focused on elucidating the precise mechanisms through which TIM-3 influences microglial behavior and its overall impact on brain health. The discovery of compounds capable of inhibiting TIM-3 function could mark a pivotal change in how Alzheimer’s is treated, transitioning from symptomatic relief to direct intervention in disease mechanisms.
Collaborative efforts among research institutions, like those led by prominent figures in the field, are fostering innovation. By employing advanced methodologies, these teams seek to explore the clinical applications of their findings, with hopes of initiating human trials that could validate the effectiveness of TIM-3 targeted therapies. Success in this area could provide new hope for millions affected by Alzheimer’s disease, potentially transforming patient outcomes in the process.
Potential of Gene Therapy in Alzheimer’s Treatment
Gene therapy represents an exciting prospect for Alzheimer’s treatment, aiming to modify genetic expressions that contribute to disease pathology. Given that the TIM-3 gene has been linked to increased risk and severity of Alzheimer’s, strategies to modulate its expression may provide novel avenues for intervention. By potentially silencing or altering the activity of the TIM-3 gene in specific populations, researchers hope to restore normal immune functions in the brain and improve cognitive outcomes.
As research progresses, integrating gene therapy with existing immunotherapy approaches could create a multifaceted treatment plan that addresses both the root causes of Alzheimer’s disease and its symptoms. Such synergies may enhance the overall effectiveness of therapeutic interventions, leading to significant strides in managing this complex neurodegenerative disorder. Ongoing clinical and preclinical studies will be essential in navigating this path forward.
Future Directions for Alzheimer’s Research
The future of Alzheimer’s research is set to focus increasingly on the intersection of immunology and neurobiology, particularly through the lens of immune checkpoint molecules like TIM-3. As scientists uncover more details about the mechanisms linking the immune system’s function to Alzheimer’s pathology, new therapeutic options will likely emerge. These could include the development of small molecules or biologics that not only inhibit TIM-3 but also enhance microglial efficacy, facilitating the removal of harmful plaques.
With an emphasis on personalized medicine, future research will also explore how genetic differences among Alzheimer’s patients influence treatment responses. This understanding could pave the way for tailored interventions that are more effective for particular patient demographics, enhancing the standard of care for those battling Alzheimer’s. Through continued collaboration and innovation, the scientific community aims to conquer Alzheimer’s disease, offering hope to patients and families affected by this devastating condition.
Frequently Asked Questions
What is TIM-3 therapy for Alzheimer’s disease?
TIM-3 therapy for Alzheimer’s disease involves targeting the TIM-3 checkpoint molecule, which inhibits brain immune cells called microglia from clearing amyloid plaques. By using anti-TIM-3 antibodies or small molecules to block TIM-3’s function, this therapy aims to enhance plaque removal and potentially improve cognitive functions affected by Alzheimer’s.
How does TIM-3 therapy improve cognitive function in Alzheimer’s patients?
TIM-3 therapy improves cognitive function in Alzheimer’s patients by allowing microglia to regain their ability to clear amyloid plaques, which are detrimental to brain health. In studies, mice treated with TIM-3 inhibitors showed reduced plaque burden and improved memory performance, indicating a potential pathway for cognitive function enhancement in humans as well.
What role do microglia play in TIM-3 therapy for Alzheimer’s disease?
In TIM-3 therapy for Alzheimer’s disease, microglia are the key immune cells that remove harmful plaques from the brain. By inhibiting TIM-3, these cells can effectively engage plaques and restore cognitive function, showcasing the critical importance of microglial activation in combating Alzheimer’s.
What are the potential benefits of using anti-TIM-3 antibodies in Alzheimer’s treatment?
The potential benefits of using anti-TIM-3 antibodies in Alzheimer’s treatment include the ability to reduce amyloid plaque accumulation in the brain, improve cognitive functions, and establish a new therapeutic strategy after previous failures in Alzheimer’s drug trials.
How does TIM-3 expression differ between healthy individuals and Alzheimer’s patients?
TIM-3 expression is significantly higher in microglia from Alzheimer’s patients compared to healthy individuals. This overexpression prevents microglia from effectively clearing amyloid beta plaques, leading to cognitive decline.
What specific genetic link does TIM-3 have with Alzheimer’s disease?
TIM-3 is linked to Alzheimer’s disease through a polymorphism in the HAVCR2 gene, which has been associated with increased risk of late-onset Alzheimer’s. This connection indicates a genetic vulnerability related to TIM-3’s function in immune response and plaque clearance.
What research has been conducted on TIM-3 and Alzheimer’s at Harvard Medical School?
Research at Harvard Medical School, led by Vijay Kuchroo, demonstrated that deletion of the TIM-3 gene in mice enhances microglial activity, allowing for better clearance of amyloid plaques and resulting in improved cognitive behaviors, highlighting a promising avenue for Alzheimer’s treatment.
How long did the research on TIM-3 therapy for Alzheimer’s take?
The research on TIM-3 therapy for Alzheimer’s took approximately five years, involving extensive collaboration and experimentation to understand the role of TIM-3 in microglial function and plaque clearance in mouse models.
What challenges does TIM-3 therapy address in Alzheimer’s treatment?
TIM-3 therapy addresses challenges in Alzheimer’s treatment by focusing on enabling effective immune responses through microglial engagement with plaques, overcoming limitations seen in previous anti-amyloid treatments that often did not reach the brain effectively.
What are the next steps for TIM-3 therapy research in humans?
The next steps in TIM-3 therapy research involve testing human anti-TIM-3 antibodies in mouse models that replicate human Alzheimer’s conditions to evaluate their effectiveness in halting plaque development and improving cognitive outcomes.
| Key Points | Details |
|---|---|
| Study Purpose | To explore the potential of TIM-3 therapy for treating Alzheimer’s disease by utilizing immune system strategies used in cancer treatment. |
| Research Findings | Deletion of TIM-3 allows microglia to clear amyloid plaques in the brain, resulting in improved cognitive function in mice. |
| Importance of TIM-3 | TIM-3 is a checkpoint molecule that normally inhibits immune responses, but its overexpression in Alzheimer’s patients prevents microglia from attacking harmful plaques. |
| Microglia Role | Microglia are crucial brain immune cells that remove debris and prune synapses, but their function is hindered by TIM-3 in Alzheimer’s. |
| Potential Treatment | Proposed methods include anti-TIM-3 antibodies or small molecules that inhibit TIM-3’s functions, enhancing microglial activity. |
| Future Research | Currently investigating the use of human anti-TIM-3 antibodies in animal models to see if they can halt plaque development. |
Summary
TIM-3 therapy for Alzheimer’s is a groundbreaking approach that harnesses the strategies used in cancer treatments to potentially combat Alzheimer’s disease. Recent studies reveal that by inhibiting TIM-3, microglia can effectively clear toxic plaques from the brain, significantly boosting cognitive functions in model organisms. This innovative strategy opens up new avenues for Alzheimer’s treatment, offering hope where traditional therapies have failed.